Bridging the Divide Between Global Mental Health Treatment Gap and Global Healthcare Reality
Table of Contents
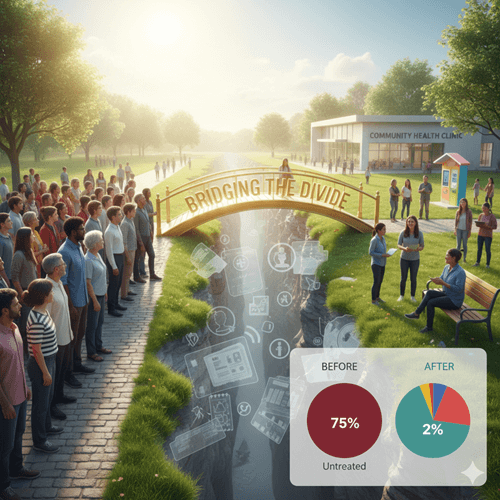
In 2026, we find ourselves at a critical crossroads in global healthcare. While awareness regarding mental wellness has reached an all-time high, the actual delivery of services remains stuck in a cycle of historical neglect and systemic inequality. The World Federation for Mental Health highlights a staggering reality: mental health is often under-prioritized, creating massive treatment gaps that deprive millions of the right to live with dignity.
Whether you are navigating a career change or managing the stresses of modern parenting, understanding the landscape of mental health equity is essential. The gap between those who can access care and those who are left behind is not just a medical issue—it is a social injustice.+1
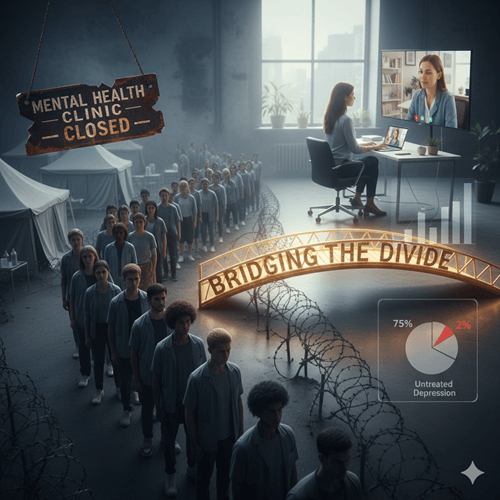
The Grim Reality of the Global Mental Health Treatment Gap
The “Global Mental Health Treatment Gap” refers to the percentage of people who need mental health care but do not receive it. Even in a world that is more connected than ever, these numbers are sobering:
- In Low- and Middle-Income Countries (LMICs): Between 75% and 95% of people with mental disorders are unable to access any mental health services at all.+1
- In High-Income Countries: Access is not significantly better; nearly 75% of people suffering from depression report not receiving adequate care.
- Budgetary Disparities: Governments worldwide spend, on average, just over 2% of their total health budgets on mental health.+1
- International Aid: Development assistance for mental health has historically never exceeded 1% of total health-related assistance.
Why the Global Mental Health Treatment Gap Persists: Social Determinants and Inequality
Inequality in Global Mental Health Treatment Gap is not just about a lack of doctors; it is deeply rooted in the conditions in which people are born, grow, and live. According to the World Health Organization, these “social determinants” include:+3
1. Poverty and Economic Turmoil
Poverty is often described as the world’s most ruthless killer and the greatest cause of suffering. The socio-economic impact of the COVID-19 pandemic has further widened the gap between the “haves” and “have-nots,” leaving those in poverty with virtually no safety net.+2
2. Stigma and Discrimination
Stigma remains a primary barrier to seeking help. It affects not just the individual’s mental state, but also their educational opportunities and job prospects. This is particularly true for marginalized groups based on race, ethnicity, and gender identity.+4
3. Fragile Humanitarian Settings
People caught in armed conflicts or natural disasters face a massive increase in mental health conditions, with prevalence rates estimated at 22%. Yet, these are the areas where health systems are most likely to be overwhelmed.+3
Moving from Evidence to Action: Scaling Up Access
To make mental health care for all a reality, we must shift our strategy from institutionalized care to community-based solutions. For more insights into how professional discipline and strategic planning can impact global systems, you can explore the resources at anshshrivastava.com.+1
The Integrated Care Model
Integration of Global Mental Health Treatment Gap into primary care is the most inclusive and efficient approach. By training family doctors and community health workers, we can provide care where people already live and work.+2
Universal Health Coverage (UHC)
Mental health must be a funded priority within Universal Health Coverage plans to ensure services are free or affordable at the point of care. Without financial risk protection, the most vulnerable continue to pay out-of-pocket, pushing them deeper into poverty.+2
Conclusion
Mental health is everyone’s business. The global treatment gap is a reminder that while we have the scientific tools to treat mental illness, we still lack the political and economic will to distribute those tools equitably. By advocating for increased investment and rights-based legislation, we can create a world where every citizen is protected and respected.+3
Frequently Asked Questions
Why is mental health care so expensive in some countries?
In 43% of African countries, for example, people pay mostly or entirely out-of-pocket due to a lack of government subsidies.
Can primary care doctors really treat mental illness?
Yes. Studies in countries like India and Nigeria show that simply trained general health workers can help many of those affected by mental illness.
How did COVID-19 affect mental health inequality?
The pandemic exacerbated poverty and food insecurity, which in turn adversely influenced population mental health, particularly in LMICs.+1
What is the impact of “Brain Drain” on mental health?
Over a third of medical graduates from some regions leave for high-income countries, leaving their home nations with as few as 0.3 psychiatrists per 100,000 people.+1
What is the “Friendship Bench” model?
It is a successful, low-cost intervention using trained “grandmother” counselors to provide mental health support in community settings, significantly reducing symptoms of depression.+1